March 2022

WELCOME, TENA KOUTOU KATOA, KIA ORANA, TALOFA LAVA, MALO LELEI, FAKAALOFA ATU.
Editorial
The latest Report on Maternity published annually by the Ministry of Health shows that from 2009 to 2019 (the latest report available), home was the place of birth for consistently only around 3.5% of births. I say “only” because AotearoaNZ is fortunate to have a maternity system in which home birthing is well integrated and LMC midwives are willing to support this option are available in most regions.
MSCC has consistently attempted to encourage women to believe in their innate ability to grow, birth and nurture their babies. Many first time mothers tell us that they have chosen to birth in a hospital “just in case”. Previous MSCC newsletters have reported that even low risk women who birth in a Level 2 or 3 hospital and supported by an LMC midwife, are exposed to multiple medical interventions. These experiences seem to further undermine women’s confidence in physiological birth and pretty much ensure that they will believe that they need to birth any subsequent children in the hospital setting.
Since second wave feminists demanded respect for women’s reproductive rights and choices (including the option of home birth), 50 years ago, research enquiring into the “safety” of homebirth has been published regularly and debated (sometimes hotly) in maternity, obstetric and public health settings, locally and internationally. In contrast, maternity outcomes published in various annual reports in AotearoaNZ over the past few decades, like the “Maternity Clinical Indicators” (discussed in our last newsletter), the National Women’s Health Annual Clinical Report, our national annual Report on Maternity, show a year on year reduction in the percentage of women experiencing a spontaneous vaginal birth – a fact that has failed to spark any significant public or professional debate.
In this edition we look at data from the latest annual Report on Maternity, data suggests that we should instead be asking;
“Is hospital birth safe for most women and their babies?”
Thanks to Hallie Campbell, nzbirthstories.com and the whanau pictured for use of the image above.
Home Birth in AotearoaNZ
In well-resourced countries birth has become the most common reason for hospital admission. With the exception of the Netherlands, only a tiny percentage of pregnant women choose and are supported to birth at home. In AotearoaNZ, all pregnant women are supposed to be informed about all their options for place of birth early in their pregnancies. Information on the findyourmidwife.co.nz website indicates that approximately 65% of LMC midwives are willing to provide care to women/whanau choosing to give birth at home. While the homebirth option is accepted and integrated into our maternity system, the belief that hospital birth is “safer”, together with a lack of confidence in women’s ability to birth physiologically that appears to have increased amongst women and maternity care providers, means that fewer that 5% of mothers/parents-to-be in AotearoaNZ choose to birth at home.
Ministry of Health NZ – Annual Reports on Maternity
In AotearoaNZ, it is impossible to get information about the health status of the women who plan homebirths, the rate of transfers to hospital or the outcomes for either mothers or babies from our Ministry of Health’s annual Report on Maternity or any other official source. The Report on Maternity publishing (a little) national maternity data for 2018 & 2019 was (finally!) uploaded on the Ministry of Health’s website in November 2021[1]. Unfortunately, it seems that these annual reports have now abandoned any written analysis or discussion of the data and provide only very basic statistical information. MSCC wonders why such a basic report takes at least 2 years to be published? An early opportunity to analyse 2020 maternity outcomes for mothers and babies during the first wave of the pandemic response would surely have been useful when deciding on how the service would respond when the virus was circulating again in the community during 2021 and 2022. Anecdotal reports tell us that more women opted for homebirth during the Lockdowns in both 2020 and 2021, however it seems that we’ll have to wait a few years before the extent of this increase is confirmed and a few more years before we will be able to determine if an increase during times of pandemic restrictions has had a more lasting impact on the numbers of women/whanau choosing to give birth at home in AotearoaNZ.
1] https://www.health.govt.nz/publication/report-maternity-web-tool

Thanks to Hallie Campbell, nzbirthstories.com and the whanau pictured for use of this image
So, what does this annual Report on Maternity tell us about place of birth in general and home birth in particular?
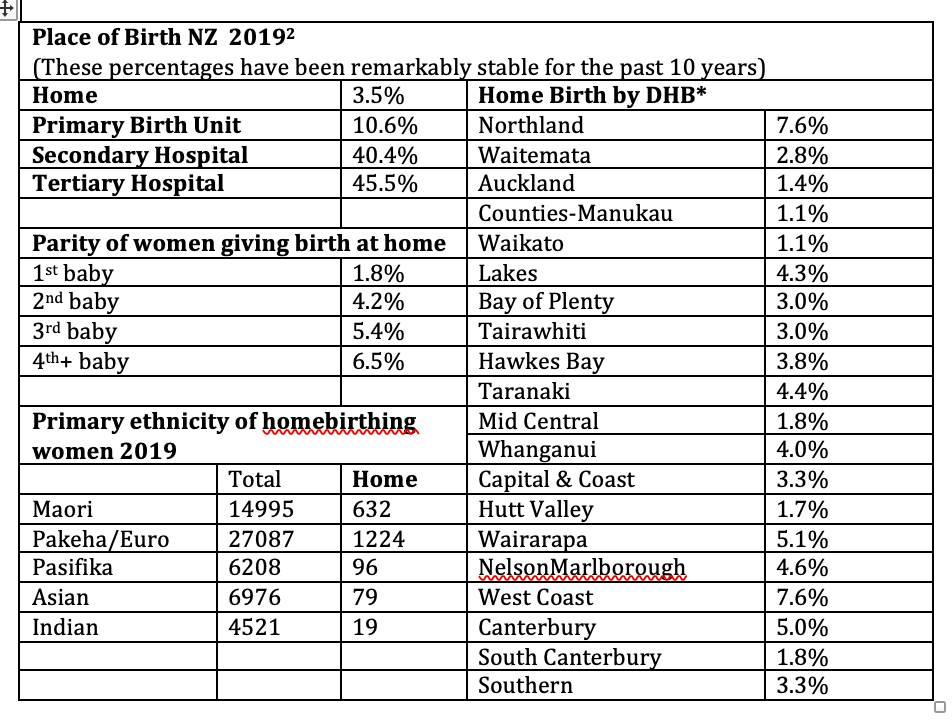
*The Report does not tell us whether this percentages in this table represent women who plan to birth at home or whether it is the percentage of women who actually birth at home. This report states the obvious; that 100% of women who birthed at home had a spontaneous vaginal birth, but it fails to give us any information about either the percentage who transferred from home to hospital in labour or the outcomes for these mothers and babies – information that many women/whanau considering home birth need to inform their choice of birth place.
2] https://www.health.govt.nz/publication/report-maternity-web-tool
Is Hospital Birth Safe for mothers?
Many parents cite “safety” as their primary motivation for rejecting homebirth (and birth in a Primary Maternity Unit). Many indicate anxiety around the perceived delays and discomfort associated with the possible need to transfer to hospital from home.
With statistics published in this latest Report on Maternity 2019 confirming a trend of increased intervention, MSCC encourages birthing whanau to consider whether our hospitals really are safe places for most women to birth in. Nationally only 59.8% of women had a spontaneous vaginal birth (SVB) in 2019, a rate that has steadily declined since 2009 when 67% of women birthed vaginally. As could be expected, the reduction in SVBs has been accompanied by an annual increase in the caesarean section rate from 24.3% in 2009 to 29.1% in 2019.
One would have hoped that the percentage of forceps or ventouse assisted births might have decreased as caesarean rates increased, instead there has been a slow but steady increase in the percentage of instrumental births during the past decade from 18.71% in 2009 to 20.73% in 2019. Likewise, despite a reduction in the vaginal birth rate, episiotomy rates have risen during this time from 12.3% in 2009 to 16% in 2019.
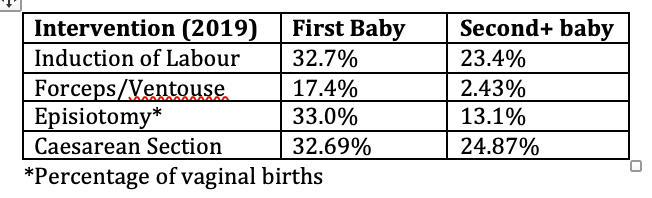
All-in-all the risks associated with hospital births especially for women having their first babies seem pretty high.
Some women who plan to birth at home will also experience these interventions, but this annual Report on Maternity does not provide sufficient data to compare any outcomes for mothers and babies by planned place of birth. Anybody looking to our Ministry of Health for data to inform their choice of place of birth will be left with lots of questions.
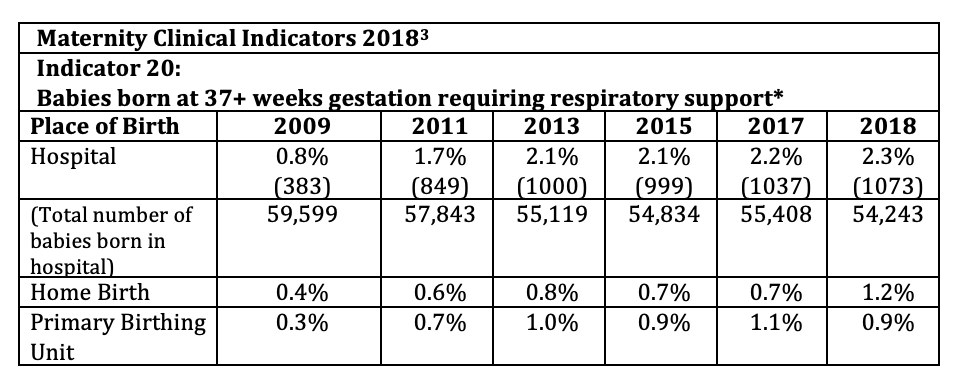
Is Hospital Birth safe for babies?
Unfortunately, the annual Report on Maternity provides no newborn morbidity data at all! The annual Maternity Clinical Indicators Report (latest available data is for 2018!) measures only one indicator that could suggest morbidity related to place of birth for fullterm babies:-

Indicator 20: Babies born at 37+ weeks gestation requiring respiratory support.
[3] https://www.health.govt.nz/publication/new-zealand-maternity-clinical-indicators-2018
Unfortunately, the publicly available maternity statistics give us no real indication of whether home or hospital birth provides better outcomes for babies. It would be useful if the annual Maternity Clinical Indicators report drilled down into this by reporting on morbidity rates/numbers for babies born to low risk first time mothers (standard primips), for type of birth e.g. vaginal births, instrumental births, caesarean sections and planned place of birth at the onset of labour.
Have you considered a home birth?
Birth has become the most common reason for hospital admission in well-resourced countries[5]. The option of home birth is well-integrated into the provision of maternity services in some countries, including AotearoaNZ. (i.e. midwives are trained to support and legally able to offer home birth, protocols for transfer of mother and/baby to hospital from home are established.) Controversy about the safety of home birth persists and increasingly women and their caregivers eliminate this option because of perceived risks and a growing lack of confidence in women’s ability to give birth without medical assistance or at the very least, medical back up “on hand”. These concerns are not backed up by good quality recently published research.
[5] Hutton EK, Reitsma A, Simioni J, Brunton G, Kaufman K. Perinatal or neonatal mortality among women who intend at the onset of labour to give birth at home compared to women of low obstetrical risk who intend to give birth in hospital: A systematic review and meta-analyses. EClinicalMedicine. 2019;14:59-70.
Home Birth in AotearoaNZ
Place of birth and outcomes for a cohort of low risk women in New Zealand: A comparison with Birthplace England.
Published: NZCOM Journal Dec2014, Issue 50, p11-18. http://dx.doi.org/10.12784/nzcomjnl50.2014.2.11-18
Although this 2014, NZ retrospective study, was designed to compare local place of birth outcomes with those reported in a 2011 British study, the data provides recent and comprehensive statistics related to planned place of birth for low risk women, receiving continuity of maternity care from an LMC midwife in AotearoaNZ.
The majority of LMC midwives submit statistics to the New Zealand College of Midwives Clinical Outcomes Research Database (NZCOMCORD). This study analysed NZCOMCORD data related to 61,072 low risk women who gave birth from 2006 -2010 inclusive.
In a statement that resonates strongly in 2022, the authors state, “The decision to birth at home is culturally and socially driven and is often considered challenging when the default place of birth is a hospital setting. The provision of homebirth as a choice of birth setting requires both that women have autonomy and rights over their bodies and that midwives have autonomy to advocate for women and support homebirth.”
Low risk was defined as, having a singleton baby in a head down position (cephalic presentation) who established in labour after reaching 37 weeks of pregnancy. Women who had an unplanned homebirth, a planned c-section, a BMI of >35 or medical or obstetric risk factors were excluded.

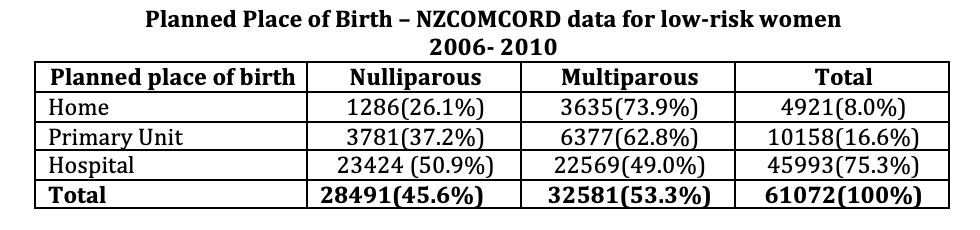
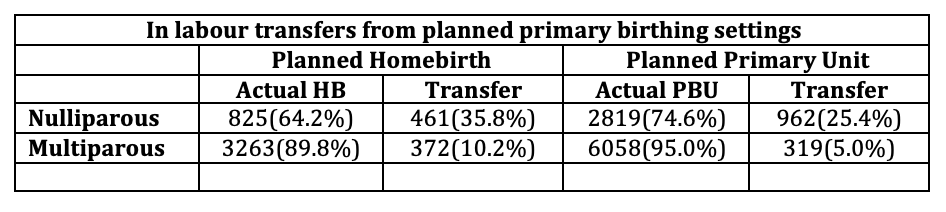
Transfer to Hospital
The table above tells us that less than 25% of low-risk women receiving continuity of care from an LMC midwife chose to birth in a primary setting. Anecdotally we are aware that many women/whanau reject homebirth because they worry about the need for an emergency transfer to hospital. In fact, only a tiny percentage of transfers from either a planned homebirth or a planned Primary Birthing Unit birth are emergencies. The majority are for much more mundane reasons like slow progress and/or maternal request for medical pain relief, both of which are more likely to occur during a first labour. When discussing the option of homebirth or birthing in a PBU, women need to consider that all planned hospital births involve a transfer to hospital in established labour. Women planning a homebirth are aware that transfer to hospital may be necessary and are always advised to have a “hospital bag” packed to make a possible hospital transfer easier and less stressful.
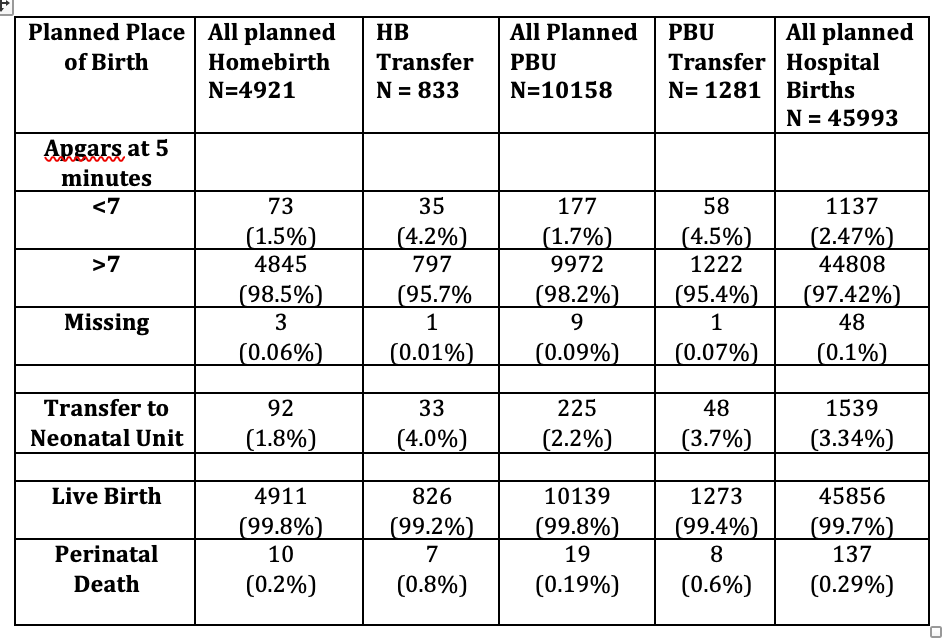
Neonatal outcomes
The incidence of adverse outcomes, such as Apgar score less than seven at five minutes, admission to a neonatal unit and perinatal mortality were low as would be expected in a cohort of low risk women, regardless of planned birthplace. However, perinatal outcomes for babies of women transferred during labour were not as good as for those who were born where planned. The authors suggest that this possibly shows, “appropriate transfer to hospital of women or babies who need referral owing to complications arising during labour…” They go on to say that, “Further research is needed focused on women who transfer during labour and whether continuity of midwifery care continues after transfer, to determine the potential impact this may have on maternal and neonatal outcomes.”
Is Home Birth safe for women with risk factors?
Women are often told or assume, that home birth is not an option for them because they have a pre-existing medical or obstetric condition/or history or because they develop one or more of what are considered to be “risk factors “during their current pregnancy. Individuals assess risk differently and have different levels of risk tolerance. In general, our medical model of maternity care manages for the worst case scenario. Individual women and their maternity care providers will often assess risk more wholistically and include a much broader range of variables in their assessment. Midwifery led research acknowledges that some women with risk factors will choose to give birth at home and some maternity care providers, mostly midwives, will support this choice.
Perinatal and maternal out comes in planned home and obstetric unit births in women at ‘higher risk of complications: secondary analysis of the Birthplace national prospective cohort study.
Published:British Journal of Obstetrics and Gynaecology 2015;122:741-753.
https://obgyn.onlinelibrary.wiley.com/doi/pdf/10.1111/1471-0528.13283
This secondary analysis of the Birthplace (2011) study compared outcomes for 8180 higher risk women, 6691 of whom planned to birth in a hospital and 1489 who planned to birth at home. Women in the planned home birth group were matched as closely as possible with women in the planned obstetric unit group.
Maternal risk factors included:-
- Medical conditions e.g. hypertensive disorders, diabetes, epilepsy, Group B strep positive
- Obstetric history e.g. previous caesarean section, postpartum haemorrhage or retained placenta
- Conditions present in the current pregnancy e.g. pre-eclampsia or pregnancy induced hypertension, gestational diabetes, BMI >35 kg/m2 at booking, gestation >42 weeks, small for gestational age
Understandably, apart from BMI>35kg/m2 and post-term pregnancy, all complications were more common in the group planning to birth in an obstetric unit (OU) and because more women in the planned hospital birth group had more than one risk factor and other complicating conditions at the onset of labour, the matching of women in the two groups was complicated. Even after adjusting for these differences however, the ‘higher risk’ women, who planned a home birth had a significantly reduced risk of mortality and morbidity, and a lower rate of admission of their babies to a neonatal unit at < 48 hours old for more than 48 hours, than the women with similar risk factors who birthed in a hospital.
The women with one or more risk factor who planned a homebirth (including the 39% of first-time mothers and 14% of multiparous women who were transferred to hospital during labour or in the immediate postnatal period) also experienced significantly fewer medical interventions during labour, fewer adverse maternal outcomes requiring obstetric care and were much more likely to experience a straightforward vaginal birth than the matched group of women who planned to birth in a hospital.
Home Birth after Caesarean Section (HBAC)
During the past 40 years there has been a steady rise in the percentage of babies born by caesarean in most countries of the world. In AotearoaNZ most obstetricians and District Health Boards consider that women who have had a previous caesarean have a risk factor that requires them to give birth in a secondary or tertiary hospital (and most DHBs also have policies that prevent a woman with a history of c-section from birthing in a DHB owned and administered PBU even when the woman’s LMC is prepared to support this choice). Every year, a small number of women who are determined to increase their chances of a vaginal birth after caesarean (VBAC) by avoiding the often restrictive hospital protocols for VBAC (usually involving multiple routine interventions and time limits on the duration of the stages of labour) choose a home birth after caesarean (HBAC).
A Canadian study published in 2021 compares outcomes for home and hospital VBACs. (British Columbia has a similar midwifery model to that in AotearoaNZ i.e midwives caseload and are mandated to offer the option of home or hospital birth to their clients.)
Perinatal outcomes of planned home birth after caesarean and planned hospital vaginal birth after caesarean at term gestation in British Columbia, Canada: A retrospective population-based cohort study.
Published: Birth, September 2021, 48:3;301-308. https://doi.org/10.1111/birt.12539
“The aim of this retrospective population-based cohort study was to determine whether the mode of delivery and maternal and neonatal outcomes differ between planned home VBAC(HBAC) and planned hospital VBAC.

This study included 4741 women who birthed between 2000 and 2017, had had at least one previous caesarean birth and planned a VBAC or a HBAC. All these women were considered healthy and met low risk criteria for VBAC eligibility. There were no significant differences between the two groups with respect to the maternal age, number of previous caesarean births, history of mental health problems, substance use or smoking during pregnancy. The percentage of women with pre-existing health conditions or pregnancy complications was significantly lower in the planned HBAC group than in the VBAC group and the percentage who had experienced a previous vaginal birth was also higher in the HBAC group. After adjusting for these factors and other relevant confounders, the study authors found no significant differences in the rate of adverse outcomes.
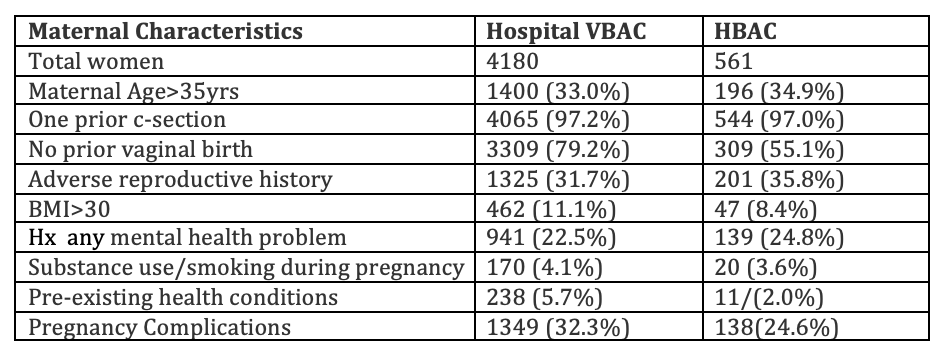
Severe adverse outcomes for mothers or babies were uncommon in both groups. The outcomes for babies were similar in both groups with very few babies requiring admission to NICU or neonatal resuscitation. However, women who planned HBACs had significantly lower rates of medical intervention in labour and showed significantly lower odds of caesarean birth compared with those who planned hospital VBACs.
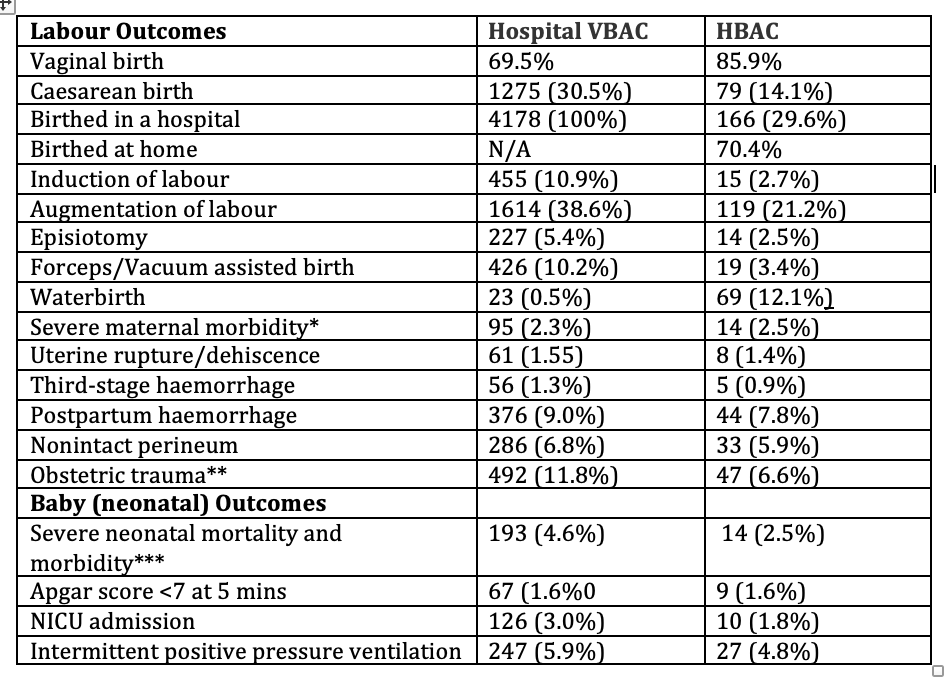
**3rd or 4th degree perineal tears, cervical tears, high vaginal tears, uterine rupture/dehiscence or inversion, pelvic haematoma, organ damage, joint/ligament damage during delivery
*** although the incidence of neonatal mortality and severe morbidity were significantly lower among those who planned home births, after adjustment for potential confounders, there was no significant association between the place of birth and these neonatal outcomes
The authors concluded “Home births for those eligible for VBACs and attended by registered midwives within an integrated health system were associated with higher vaginal birth rates compared with planned hospital VBACs.”
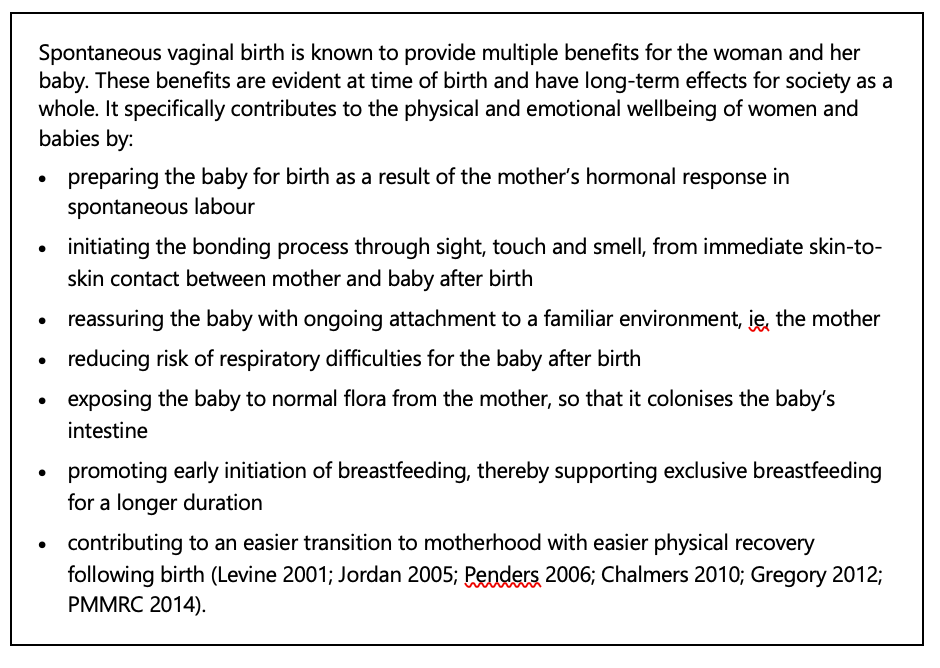
VBAC in AotearoaNZ
Our MoH’s Annual Report on Maternity 2019 does not provide VBAC statistics or any other mention of VBAC, perhaps signalling that our health authority is not concerned about the continuing increase in the rate of c-section birth? We were unable to find any national data about VBAC. However, the last narrative form Annual Report on Maternity 2017, does describe the benefits of vaginal birth for mother and baby.[6]
[6] https://www.health.govt.nz/publication/report-maternity-2017
Planned Home Birth Safety vindicated by recent large studies
The quality of research into home birth has improved dramatically since midwives became involved in designing and analysing home birth studies. Two large systematic reviews and meta-analyses of data comparing planned homebirth outcomes for mothers and their babies with outcomes for low-risk women planning hospital births, published in 2018 and 2019, should encourage health officials from government to clinical level and maternity care providers to promote and support the homebirth option.
Maternal and perinatal outcomes by planned place of birth among women with low-risk pregnancies in high-income countries: A systematic review and meta-analysis.
Published: Midwifery 2018;62:240-255 https://doi.org/10.1016/j.midw.2018.03.024
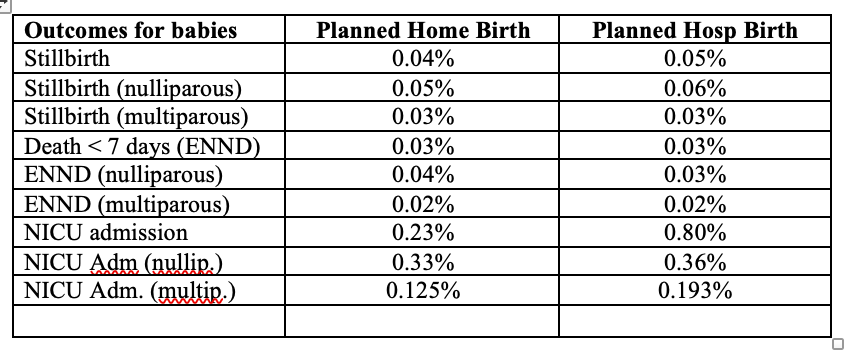
This review compared “outcomes by place of birth among women with low risk pregnancies in high-income countries[1]” (including NZ). Twenty-eight studies published between 2000 and 2016, that met clearly defined criteria for healthy women, low risk pregnancy and intended place of birth at the onset of labour, were included in these meta-analyses..
[1] As defined by the World Bank in 2016 http://data.worldbank.org/about/country-and-lending-groups#High_income
Some critics (reluctantly) acknowledge that planned homebirth usually results in a favourable experience for mothers e.g.significantly higher incidence of normal vaginal birth and reduced incidence of medical interventions as well as a high rate of maternal satisfaction with the birth, but have continued to hold and disseminate the view that home birth is risky for babies. This meta-analysis found no significant differences in the odds of intrapartum stillbirth or neonatal death (babies 0 – 7 days) according to place of birth, for either first time mothers or those who had already given birth. Babies born at home had significantly lower odds of NICU admission than those whose mothers planned a hospital birth. A further meta-analysis showed that there was no significant difference in odds of babies being admitted to NICU for babies of first time mothers regardless of place of birth, however the odds of NICU admission for babies of mothers who had previously given birth (multips) was significantly lower amongst planned homebirth cohorts.
[7] As defined by the World Bank in 2016 http://data.worldbank.org/about/country-and-lending-groups#High_income
Maternal Outcomes
The most striking outcome was that 90.5% of 45,777 women who planned toggle birth at home compared with 54.4% of 300,507 low risk women who planned to give birth in a hospital had a normal vaginal birth. (The metanalysis of studies comparing outcomes for women who planned to give birth in a Primary Birthing Unit and those who planned a hospital birth showed a 83.7% and 61.71% vaginal birth rate respectively.)
Women planning homebirths had significantly lower rates of caesarean section (2.14% cf 9.68%) and instrumental birth (5.71% cf 14.32%) compared with matched low-risk women who planned to birth in a hospital. Homebirthing women also experienced a lower incidence of severe perineal trauma and postpartum haemorrhage.
Perinatal or neonatal mortality among women who intend at the onset of labour to give birth at home compared to women of low obstetrical risk who intend to give birth in hospital: A systematic review and meta-analyses.
Published:The Lancet 2019;14:59-70. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6833447/
This systematic review and meta-analysis included 17 studies in the systematic review and 14 studies in the meta-analyses and focused on outcomes for babies related to place of birth. All included studies were published between 1996 and 2017 and collectively reported perinatal or neonatal outcomes for approximately 500,000 intended home births making it the largest and most comprehensive meta-analysis comparing outcomes of intended home and hospital births to date.
The authors hypothesised that the degree of integration of the home birth option and home birth practitioners within the maternity care system of different countries would impact outcomes so they conducted separate analyses for what they termed “well-integrated” and “less well integrated” homebirth services. A “well-integrated” setting was described as states/provinces/countries where home birth practitioners: are recognised by statute within their jurisdiction; have received formal training; can provide or arrange care in hospital; have access to a well-established emergency transport system; and carry emergency equipment and supplies. Less well-integrated settings were those where one or more of these criteria was absent. Thirteen studies took place where midwives attending home birth were considered to be well-integrated into the healthcare system (The Netherlands, England, Iceland, Canada, USA, New Zealand). Four studies took place in settings where midwives attending home birth were considered to be less well-integrated into the healthcare system (Norway, Sweden, Japan, Australia).
Planned Home Birth unequivocally safe for babies
This huge review and meta-analysis showed that for babies of women who intended to give birth at home when labour started, there was no increase in perinatal and neonatal mortality or morbidity compared to babies of low risk women who intended to give birth in a hospital. Meta-analysis also showed no differences in other neonatal outcomes including NICU admission, Apgar scores, or the need for resuscitation. When nulliparous and multiparous women were separated, meta-analysis found that an Apgar score of <7 at 5 min and newborn admission to NICU occurred significantly less frequently amongst babies born to multiparous women in settings where home birth and midwives were well-integrated into the maternity services when compared to babies of low risk multiparous women who planned a hospital birth.
Separate analyses found no excess of perinatal or neonatal mortality for planned home births compared with birth outcomes for babies of low-risk women who planned to birth in a hospital regardless of whether the mother was birthing a first or subsequent baby.
The reviewers concluded that, “The risk of perinatal or neonatal mortality was no different when birth was intended at home or in hospital” and added that this comprehensive study provides much needed information to assist policy makers, care providers, women and families to make informed decisions about home birth.

A culture of homebirth – three births at home
ONE
My first clear childhood memory is the home birth of my baby brother when I was 2 years old. I recall an exciting, fun and exhilarating evening as family members gathered anticipating the new arrival. Although I’m sure my mother felt a lot of that, I was blissfully unaware of all the other things she would have been experiencing! When I was six years old I was called home from a birthday party to share the joy and excitement of the home birth of my youngest sibling.
Years later when I was planning the birth of my first baby it never occurred to me that I would birth anywhere except home.
I ordered, set up and tested the birthing pool. I approached, then passed my due date. I ate pineapple, washed every car our family owned and dug my mother’s garden to encourage the onset of labour.
Eight days after my EDD, I had a show on a Sunday evening. My body gently contracted through the night, though the combination of these early labour surges and the excitement meant I got little sleep that night. The next morning things slowed and I booked in to see my midwife in the afternoon. At nine days postdates she recommended that I get a scan to check the amniotic fluid around the baby. I knew things were happening on their own so to encourage them along a bit she did a sweep of the membranes, but I took the ultrasound referral in case things didn’t progress.
An hour after this midwife visit I was in labour. Things felt like they were moving swiftly along. In the early evening my midwife joined us at our home and I felt confident labour was going in the right direction. By now I was “in the zone” changing position kneeling over the bed, lying on the bed, pacing the hallway, hanging my weight from my partner’s neck and shoulders, rocking and swaying. My movements and breathing were supported by my older sister playing the piano. I tried the pool but even with my support “team” of women singing gentle rounds and my partner rhythmically providing water massage to help me relax, I only managed to last 20 – 30 minutes in the pool. Out of the pool for more position changes with my mother leading the support team in toning to help keep my breathing rhythmic, while my sister massaged my back and legs.
My dad paced around the house inside and out in time to the humming and breathing. By midnight there was still no baby. The midwife checked my progress and found that baby’s head was deflexed (as though trying to see the way out), and posterior and I had a swollen cervical “lip”. These three things meant that although I was feeling “pushy” this baby was not going to be born for a while yet. The cervical swelling would need to disperse and my baby’s head would need to get into more favourable position.
Following my midwife’s instructions to encourage my baby to turn, I first lay on one side through as many contractions as possible, then turned on to the other side for as long as possible, then onto my hands and knees with my hips in the air and repeat! By the time the new day was dawning, after two nights of sleeplessness and labouring, I was becoming exhausted and I was still not fully dilated. My midwife hung a bag of IV fluids from the mosquito net hook to boost my energy and my mother called an acupuncturist friend to help get the baby into a more favourable position.
By the time Lisa, the acupuncturist arrived, the extra hydration had revived my focus and determination to get my baby born. Things changed quickly. I knelt leaning into the bed as my contractions got me to fully dilated. The acupuncture needles went in and with new energy after what seemed like an age of labour, in less than half an hour my baby was born.
A little girl… I lifted her into my arms and held her through the birth of the placenta. We snuggled into our bed as a new family where we ate freshly baked Birth Day cake for breakfast, admired our beautiful daughter and celebrated her birth in the same home that I’d been born in 18 years earlier.
TWO
My second baby arrived in a similar fashion. At home, 10 days after EDD and preceded by a show of blood and a full night of gentle labour before another full night of established labour – though these were about the extent of the similarities! Everyone had told me that second births were easier than the first. Boy were they wrong!
The mucous plug and blood began to come away and the prelabour contractions ramped up a full two weeks before I went into labour. I felt like labour could establish at any time and wished it would! We set up at my parent’s home on the fringes of the Waitakere Ranges and embarked on a gentle exercise regimen to encourage the onset of labour. Despite a bush walk, hill walk, or beach walk each day, my baby wasn’t ready!
Finally one Monday night I was woken by the familiar tightenings. I dozed and timed them through the night but when I got up in the morning they slowed right down again. One more bush walk!
By mid afternoon it was obvious that my baby had decided it was time. My partner began the journey back to Auckland from Glenorchy while I began the journey through the early stages of labour with my mother, father, older sister and 8 year old daughter by my side.
After hours of pacing, position change, massage with gentle cuddles and encouragement from my daughter, in the middle of the night the sensations grew stronger. The midwife and my partner arrived and helped me into the bath. I had hoped to birth my baby into the water but it didn’t quite go that way, as is often the case with birth! It became clear that once again my baby had moved into a posterior position – I knew from last time this was not ideal! I felt as though my body was trying to push my baby out but I wasn’t yet fully dilated and ready for the pushing stage.
I tried different positions in the bath, trying to relax and keep my body from pushing but after several hours, with my energy waning, my midwife encouraged me to get out of the bath. She checked me and once again I had a swollen cervical lip. By now I was quite tired so we tried almost everything to help my baby to come. We tried different positions – on and off the birthing stool, we tried rebozo, my sister massaged my aching back with heated river stones, we even tried having my midwife move the last swollen part of my cervix over my baby’s head while I contracted – I remember this as the most painful part of all my birthing experiences. Nothing worked.
A while later my baby’s heartrate showed that s/he needed to be born soon. With my family around me and now two wonderful midwives encouraging me – cheering me on even, I felt the urgency and I PUSHED. It was a completely different experience to pushing my first baby out. With my first birth I felt like I easily breathed my baby into the world, this time pushing was the most intense work I had ever done – as my mother often says “they don’t call it labour for nothing!”. I felt like I was using every muscle in my body and that my eyes might explode. Finally, the head emerged – still posterior, (no wonder it was so difficult!) Another push birthed the body completely tangled in the cord – so much so I couldn’t even bring baby to my chest. We unraveled the cord and there she was! The most beautiful 9lb baby girl I had ever seen!
As I greeted and cuddled my baby, the midwives administered syntocinon to stop the bleeding caused by the big tug on the tangled and shortened umbilical cord during her birth.
My body was exhausted and shaking, I was helped onto the bed where I birthed the placenta as I fed my new baby. When our baby fell asleep, I put her on her dad’s chest, with her sister snuggled up watching over her. Exhausted from the effort of bringing this baby into the world, I leaned on my mother as she walked me to the shower where she helped me to wash, wiping the blood from my legs as I just didn’t have the energy to even reach down – it was all I could do to stand.
THREE
I had expected baby number three to give me the same signs that it was time, but if there’s one thing you can count on with labour and birth, it’s that you never really know when or how it will unfold!
Two days before my due date I woke at 4am to a sensation that I thought was a show. I got out of bed and took a couple of steps, (clearing the carpet thankfully), as my waters broke all over the floor.
For the next four nights my body would begin to labour, then when my young daughter woke in the night it would all go quiet again! My family gathered. My midwife and I monitored myself and my baby closely. I was determined that if we were both well I wouldn’t go to hospital for an induction. I felt most comfortable birthing at home, in my familiar surroundings, with access to my things and my people and an induction in hospital would mean giving up these comforts.
On the fifth day I went to my midwife’s clinic for observation, the fetal heart monitor showed a happy baby and reasonably regular, gentle contractions. That night I walked my young daughter in the stroller around the neighbourhood, to get her to sleep, brought her home to bed and as I lay down with her, the contractions began to ramp up, just as they had done for the previous four nights but this time they kept going! At just after 2am my daughter woke, I didn’t want anything to compromise the labour so I sent her dad in to be with her and I laboured in the dark on my futon listening to music in my headphones, until I felt sure that labour was established. The contractions became longer and stronger and closer together and I phoned my mother and my older sister to come and be with me, bringing fresh energy and support… and the hot stones for lower back massage of course.
Morning (my 30th birthday) broke, my little girl got up and my contractions slowed down. I sent everyone out of the house – my partner to work, big girl to school and little girl and my nephew to the zoo with their poppa, so we women could concentrate on getting this labour to happen!
My midwife came to check on me around the middle of the day. The contractions were back, they were strong, but they were irregular. I was in labour, but it was progressing very differently to what the textbooks say. I was 4cm dilated and since my midwife had done an internal examination to determine this, I was now committed to getting this baby born. My mother, sister and midwife had a cup of tea while I had some quiet time focusing on my body.
My midwife popped into my room to say she was going to visit another client and to call her when she was needed, and said if things weren’t to progress today we would have to consider transfer to the hospital for augmentation.
Poppa and my daughter had returned exhausted, from the zoo. Poppa retired to the sleepout for a nap, my sister put my daughter in the stroller to walk her to sleep and my mother took my nephew for a bike ride to give me space to get into “the zone”… and I did.
An hour later I called both my midwife and my partner home. I sat in the shower letting the water massage my belly and back. We woke poppa and he went to get my big girl from school so that she would be home to witness her new sibling’s birth.
This time was different. This time I could feel my baby getting lower, moving through my body. I moved back to the bedroom and soon I could feel my baby coming. I felt as the head emerged and reached down and caught my baby as he was born.
Baby boy, born at the end of my bed on my birthday. The best present ever!
Sitting up in bed to birth the placenta, the afterpains came on strong! This time too there was a lot more fiddling around as some of the membranes didn’t come away – which can be a risk for infection. I’d had enough of the fiddling so I got up to shower and over the coming days did lots of stretching and abdominal massage to make sure everything came away.
These three experiences, with all their challenges and triumphs, were the best of my life.

I was raised with the belief that birth is not a medical emergency, unless it is. I was raised knowing that women are strong, and more than capable of bringing their babies into the world. It was normalised that birth doesn’t need to be feared or happen in a facility behind closed doors. That birth is a family celebration not a medical event. I know that the way I feel about birth and many of my other beliefs around my body have come from my experiences of homebirth when I was a child, as well as my own birth experiences. I hope that by sharing the experience of birth with my daughters that they will know that they too are strong and capable and can trust their bodies. And although I won’t be welcoming any more babies into our family, I hope that my son gets to witness first-hand, the power, the joy and the beauty of homebirth.
Thank you to Twyla Watson from theguthealingprotocol.com for sharing her birth stories.
Birth Stories Welcome
MSCC welcomes birth stories for publication in our newsletter and on our website. If you would like to share your birth story please send it to: [email protected]