The Maternity Services Consumer Council believes all women and their partners, families/whānau and support people should be informed and included in decisions relating to their care. This free information pack can help you navigate the choices you have and the decisions you may make during pregnancy, birth and postpartum. The pack is FREE for individuals, just pay postage.
What’s in the pack
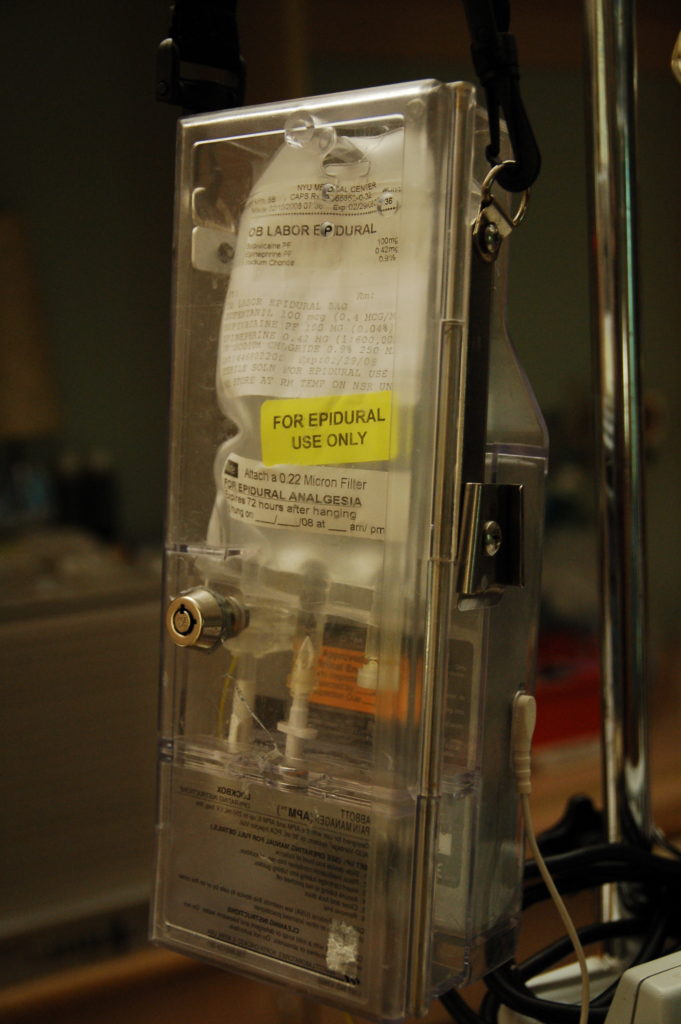
Our evidence-based, resource series for pregnant women and their whanau/families, is split into two categories – The Facts and Your Choices. This helpful and comprehensive pack contains all twelve resources from the Your Choices and The Facts ranges.
Click or tap the title of each resource for more information. Scroll down to order your free pack today!
Your Choices
If you have the ability to translate any of these resources into a language we do not have as yet available please email us at [email protected]